Contemporary Home | Events | News
This is the fortieth blog in a series on COVID-19 and lockdown, edited by contemporaryweb@rps.org and Avijit.Datta@rps.org













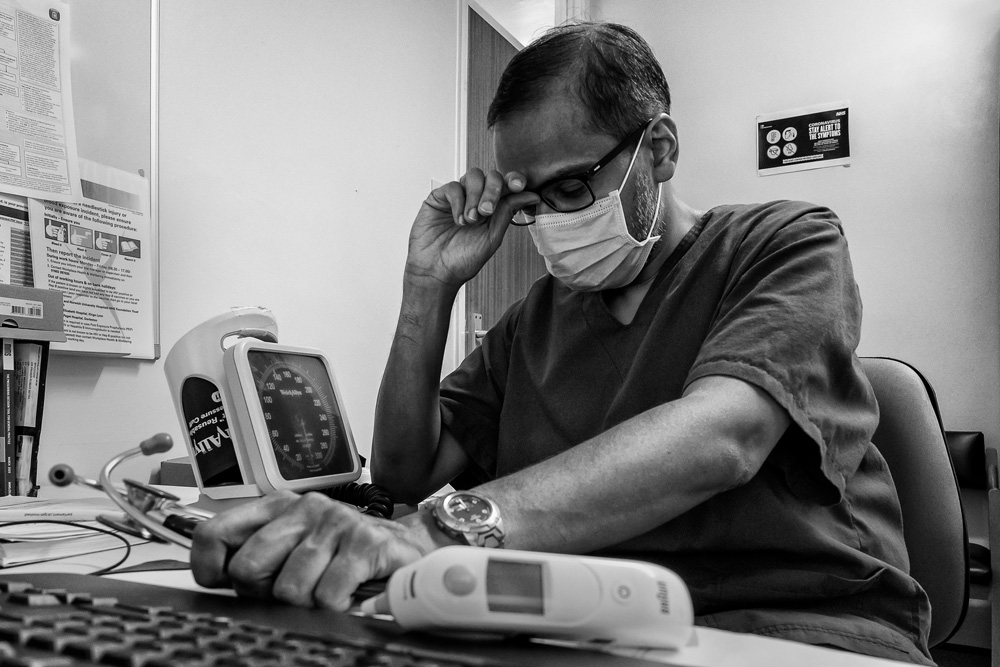
As primary care clinicians, we are often the first point of patient contact during the pandemic when COVID-19 causes havoc. We witnessed first-hand the devastating effects of the pandemic on care home residents. Media attention, including the RPS Contemporary blog series (Numbers 18, 19, 22, 23, 25, 28) had often been on hospital/ITU patients and families (QV RPS Contemporary blog by Giles Duley HonFRPS https://rps.org/news/groups/contemporary/2021/january/inside-imperial-college-healthcare-nhs-trust-icus/) but the stressful lives of residents and workers of care-homes across the country have remained largely undocumented with photography.
The carers “fought” but were poorly appreciated; they witnessed deaths at a professional and personal level almost daily. Many carers became significantly unwell with COVID and were off work whilst the remaining workforce went the extra mile to care for our loved ones.
At a time when the working population was busy, our elderly loved ones continued their silent battle against COVID-19 in care homes, being looked after by carers who became a part of their family too. The relatively low income of care home staff and their inexperience in dealing with COVID-19 did not dampen their morale, at least initially.
As hospital beds filled up fast, the care-home workforce was under pressure to minimise hospital admissions (and allegedly accepting transfers of patients from hospital) whilst ensuring the safety of residents and meeting the expectations of residents and their families. Their relatively low income and their inexperience to deal with COVID-19 could not dampen their morale.
Residents felt the heat too; their world changed dramatically. A large proportion of them could not comprehend the magnitude of the change that the outside world was going through. The residents who tested positive but could avoid hospital admissions were restricted to solitary confinement within their rooms, guarded by “butterflies” (a silent symbol used in care homes to denote COVID positive status of residents). Their mental health took a huge blow as they missed fellow residents in lounges, could not meet with family members and relied on window-visits (when allowed) and, for a handful of the technologically gifted ones, they used online platforms to communicate with their families.
The advent of vaccination (see RPS Contemporary blog https://rps.org/news/groups/contemporary/2020/december/the-fight-must-go-on/) and reliable COVID-19 testing, created a perception of hope within their world of doom and gloom. Slowly some degree of normalcy crept in when the barriers between “outside world and inside of care homes” were removed – face to face visits soon became one of the most cherished words in their dictionaries. Family members and the vulnerable care-home residents have continued to be grateful on the workforce more than ever as we still manoeuvre our way through the pandemic.
While creating this panel, as a General Practitioner, I was involved in working closely with carers, residents and their family members who have battled to safeguard a vulnerable population behind closed doors throughout the pandemic, and this represents their collective voice. I had mixed emotions while shooting the photographs – though as a doctor I am trained not to get affected emotionally with patients and their illness, I had to take care of my empathy while doing my job. The stories of the patients, their family members and the workforce of the care-homes during the pandemic nevertheless touched my heart and that is the main reason why I chose to embark on this project.
From donning PPE, to self-administering lateral flow tests prior to my visits – I took extra care to ensure that I was not increasing any risks to the people around me. I also ensured that I had written consent of staff members and patients and their family members whom I was interviewing and photographing. The managers of the care homes also had permissions from family members of patients (who were unable to consent) who were being photographed.
Editor’s Note
Dr. Mitra is a practicing NHS GP and active member of the RPS, particularly Contemporary North. His work has been published by National Geographic Traveller UK, Wanderlust UK and The Guardian and exhibited in London by Sony World Photography Awards & Travel Photographer of the Year. He has been a recipient at The Humanity Photo Awards (UNESCO and CFPA).
https://www.prabirmitra.co.uk/
This blog on Care homes during the Pandemic was published to coincide with the controversial UK Parliamentary vote on 8th September 2021 for a 1.5% planned rise in National Insurance to fund health and social care. The government claims that the majority of the funds raised by the tax rise will go towards catching up on the backlog in the NHS created by COVID-19 - increasing hospital capacity and creating space for nine million more appointments, scans and operations. A portion of the money - £5.4bn over the next three years - will also go towards changes to the social care system, with more promised after that.
The UK Office for National Statistics (ONS) published data received by the Care Quality Commission (CQC) of English care home deaths from COVID-19 at the start of the pandemic: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/numberofdeathsincarehomesnotifiedtothecarequalitycommissionengland
Between 1st Jan 2021 and 3rd September 2021, 10,534 COVID-19 deaths were recorded; the highest daily deaths was on 25th January 2021 when 459 COVID-19 deaths were recorded. The total number of care home deaths (all causes) in England in that period was 69,498. Of the 48,213 COVID-19 deaths registered in the first wave of the Pandemic, between mid-March and mid-June 2020, 40% (sic) were care home residents.
Another way of understanding the extent of the impact of COVID-19 on care home resident deaths is to look at excess deaths in care homes. Excess deaths are the number of deaths above the ‘expected number’, obtained by comparing the number of deaths from all causes with the average number of deaths over five years. Nuffield Trust analysis of ONS data showed there were 35,067 excess deaths in the first two months of the pandemic, with 6,331 deaths in the week ending 24 April alone.
Other blogs in this series:
A photobook project in 80 days
Through Our Lens COVID-19 Project
Photography and Personal Development
Photography as a tool against depression
Emotions and photography during a year of pandemic
A Buddhist Perspective on the Pandemic
Inside Imperial College Healthcare NHS Trust ICUs
Hope. Struggle. Change. March 2020 - A Lockdown Diary
‘MentalCollodion’: Supporting Mental Health with Wet Plate Photography during a Pandemic
Together we are stronger – Inside an NHS Hospital during COVID-19
Celebrating NHS Healthcare Staff in a Pandemic
Unplanned London Lockdown and Jugaad
The Covid Pandemic in Hong Kong
Fighting against stigma during COVID-19
Protesting Human Rights in a Pandemic
Go Home: Mental Stability and Collaboration in a Pandemic
Getting Through This – it’s OK not to feel OK
The New Normal and the COVID-19 Fight in India for the world
Analogue New York during protests and a pandemic
Bank Top – congregation not segregation during COVID-19